Photo by Taylor Deas-Melesh on Unsplash
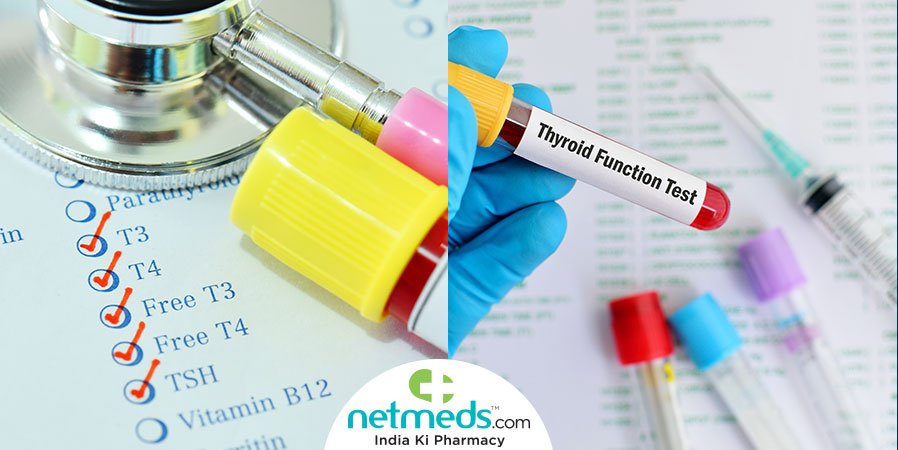
Photo by Taylor Deas-Melesh on Unsplash In iodine-sufficient areas, the most common cause of hypothyroidism is chronic autoimmune thyroiditis (also known as Hashimoto’s disease). High concentrations of anti-thyroid antibodies (predominantly thyroid peroxidase antibodies and anti-thyroglobulin antibodies) are present in most patients with autoimmune thyroiditis. Raised concentrations of thyroid peroxidase antibodies are also detected in about 11% of the general population.8 In patients with subclinical hypothyroidism, thyroid peroxidase antibody measurements help to predict progression to overt disease.23,24 The exact mechanisms underlying autoimmune thyroiditis are not known, but both genetic and environmental factors are involved. A higher genetic risk score—calculated using five genetic variants for thyroid peroxidase antibodies identified by genome-wide association studies—showed a graded association with higher TSH concentrations and clinical hypothyroidism.25,26 Smokers have lower thyroid peroxidase antibody concentrations than non-smokers, and incidence of autoimmune thyroiditis increases after smoking cessation.27,28 Other environmental factors implicated in autoimmune thyroiditis are vitamin D and selenium deficiency, and moderate alcohol intake.29
Iodine is an essential component of thyroid hormone. Iodine deficiency can result in goitre, thyroid nodules, and hypothyroidism. The most severe consequence of iodine deficiency is cretinism (ie, restricted mental and physical development in utero and during childhood). Iodine fortification programmes are one of the safest and cheapest public health interventions for the prevention of cognitive and physical impairment.30,31 Despite such efforts, suboptimal iodine status still affects large parts of Africa and Asia, as well as specific subpopulations in several high-income countries—most notably, pregnant women in some areas of Italy, USA, and the UK.31–33 In populations that shift from severe to mild iodine deficiency, the prevalence of hypothyroidism decreases; in populations shifting from mild deficiency to optimum or excessive intake of iodine, the prevalence of autoimmune hypothyroidism increases.34,35
Iodine-containing drugs (eg, amiodarone) can restrict thyroid hormone production through iodine overload, immediately blocking thyroid hormone synthesis (ie, Wolff-Chaikoff effect). About 14% of patients treated with amiodarone develop hypothyroidism.36 Lithium also causes hypothyroidism via effects on thyroid hormone synthesis and release.37 In a large population-based cohort study,38 6% of patients needed levothyroxine therapy within 18 months of starting lithium treatment. Tyrosine kinase inhibitors are used as targeted therapy for several cancers. An analysis of clinical reports from the US Food and Drug Administration Adverse Event Reporting System,39 found that patients who received sunitinib developed hypothyroidism more frequently than patients treated with sorafenib. Several other drugs—including interferon-alfa, thalidomide, some monoclonal antibodies, antiepileptic drugs, and drugs for second-line treatment of multidrug-resistant tuberculosis—can also cause primary hypothyroidism (panel).
Hypothyroidism is common after radioiodine treatment, after hemithyroidectomy, and after neck radiation or surgery for cancer therapy.40–44 In the long term, about 80% of patients with Grave’s disease who are treated with radioiodine will develop hypothyroidism, even when low doses are used. Hypothyroidism is reported to occur in 55% of patients treated for toxic nodular goitre40 and about 8% of patients treated for solitary toxic nodules.45 In a meta-analysis43 of 32 studies, 20% of patients developed hypothyroidism after hemithyroidectomy. Other causes of primary hypothyroidism include transient thyroiditis and infiltrative disease (panel).
source:www.ncbi.nlm.nih.gov
RELATED POSTS
View all